===
Read Full PDF Here
STORY AT-A-GLANCE
- Antibiotics fight bacterial infections. They have no effect on infections caused by viruses, such as the common cold, seasonal influenza, SARS-CoV-2 and some ear infections
- Antibiotic drugs are routinely overused, both in human medicine and agriculture, resulting in the proliferation of antibiotic-resistant infections
- There are many natural plant-based remedies that will help kill bacteria without the risk of building resistance
- Natural antimicrobials include medicinal honey, garlic, ginger, echinacea, goldenseal, myrrh oil, thyme essential oil, oregano oil, clove extract and cranberry juice
- Remember that upper respiratory infections (URIs) are typically caused by viruses, not bacteria, so antibiotics won’t work for these infections. For URI’s, nebulized hydrogen peroxide is one of the most effective remedies. In most URI cases, improvement is seen within a few hours
As the name implies, antibiotics help fight bacterial infections. They have no effect on infections caused by viruses, such as the common cold, seasonal influenza, SARS-CoV-2 and some ear infections. Antibiotic drugs are routinely overused, both in human medicine and agriculture, resulting in the proliferation of antibiotic-resistant infections.
Taking an antibiotic unnecessarily will also kill off your beneficial gut bacteria, which could make it more difficult for you to recover from your illness. The good news is there are many natural plant-based remedies that will help kill bacteria without the risk of building resistance. Here’s a review of 10 natural antimicrobials you can reach for as a first line of defense, before resorting to a pharmaceutical antibiotic.
Medicinal Honey
As long as you use the right kind of honey, science backs its use for a variety of bacterial infections, especially when used topically. As explained in the 2011 paper, “Honey: Its Medicinal Property and Antibacterial Activity”:1
“[The] medicinal importance of honey has been documented in the world’s oldest medical literatures, and since the ancient times, it has been known to possess antimicrobial property as well as wound-healing activity.
The healing property of honey is due to the fact that it offers antibacterial activity, maintains a moist wound condition, and its high viscosity helps to provide a protective barrier to prevent infection. Its immunomodulatory property is relevant to wound repair too.
The antimicrobial activity in most honeys is due to the enzymatic production of hydrogen peroxide. However, another kind of honey, called non-peroxide honey (viz., manuka honey), displays significant antibacterial effects even when the hydrogen peroxide activity is blocked …
The medical grade honeys have potent in vitro bactericidal activity against antibiotic-resistant bacteria causing several life-threatening infections to humans.”
In 2018, the U.K. Department of Health proposed guidelines recommending the use of honey as a first line of treatment for coughs, as part of its goal to reduce inappropriate antibiotic use. As reported by BBC News:2
“A hot drink with honey — and often with lemon and ginger as well — is a well-known home remedy for coughs and a sore throat … [P]roposed guidelines from the National Institute for Health and Care Excellence (NICE) and Public Health England (PHE) say there is some limited evidence that it can help improve cough symptoms.”
The nectar from the manuka flower contains dihydroxyacetone, a precursor to methylglyoxal (MGO), an antimicrobial compound not found in most other honey. Australian manuka honey is perhaps the most well-known and well-studied medicinal honey, with clinical studies demonstrating its effectiveness in the treatment of:3
- Bacterial infections — Manuka honey has been shown to effectively eradicate a long list of bacteria,4 including helicobacter pylori responsible for peptic ulcer diseases and gastritis, and methicillin-resistant Staphylococcus aureus (MRSA). Manuka honey also effectively removes stubborn biofilm produced by Staphylococcus aureus5
- Skin diseases, ulcers, burns and necrosis
- Dental caries and plaque, periodontal infections and gingivitis
- Ulcerative colitis and inflammatory bowel disease (IBD)
- Wounds, including post-surgical wounds
The U.S. Food and Drug Administration authorized the first manuka-based medical product in 20076 (Medihoney by Derma Sciences Inc.). Today, several different brands of Manuka-based wound and burn dressings can be found online.
Do not use conventional store-bought honey for wound care. It lacks the medicinal qualities of medicinal honeys like Manuka, and could potentially feed rather than inhibit the growth of harmful bacteria. For more information, see this September 21, 2022, article on Manuka honey. Used internally, your best bet is raw, locally sourced, unprocessed honey. There’s a lot of fake honey out there, so use caution.
Garlic
Garlic has been used to fight bacterial and parasitical infections for centuries. According to a 2014 review, garlic has been proven effective against “a plethora of gram-positive, gram-negative, and acid-fast bacteria,” including but not limited to:7
| Salmonella | Escherichia coli |
| Pseudomonas | Proteus |
| Staphylococcus aureus | Klebsiella |
| Micrococcus | Bacillus subtIlis |
| Clostridium | Mycobacterium |
| Helicobacter | Vancomycin-resistant enterococcus |
Importantly, garlic “exerts a differential inhibition between beneficial intestinal microflora and potentially harmful enterobacteria,” meaning it inhibits bad bacteria while leaving good bacteria alone.8
Garlic also has antiprotozoal and antifungal properties, and according to the 2014 review9 above, garlic can be an effective treatment for conditions such as Candida albicans, multidrug-resistant tuberculosis and giardiasis.
In the case of giardiasis — an intestinal infection marked by stomach cramps, bloating, nausea and watery diarrhea — researchers found commercially available garlic capsules eliminated the symptoms in all patients within 24 hours.
Research also supports the use of garlic and garlic derivatives for chronic external- and middle-ear infections. According to one such study,10 two components of garlic, allicin and s-allyl cysteine (SAC), were effective against the microorganisms involved in most ear infections, even at low concentrations. Garlic-infused oils are commercially available, but you can also make your own. Here’s a recipe previously published by Verywell Health:11
“You will need one garlic clove, olive oil, a pan, a strainer, a glass jar with a lid, a dropper, and a piece of cotton. You can make your own garlic oil in a few easy steps:
1.Peel and crush up the garlic.
2.Warm the oil and garlic slowly on low heat until the garlic and oil are fragrant.
3.Remove it from heat so that the mixture can cool down.
4.Strain the garlic from the oil while pouring it into a jar.
Once the oil is ready, you can use it as you would any other type of eardrop.”

Save This Article for Later – Get the PDF Now
Ginger
Ginger, available in extract, tincture, oil and oral capsule form, also has potent antimicrobial activity. A 2020 study12 demonstrated that ginger essential oil was effective against E. coli and S. aureus, two bacteria involved in periodontal infections.
According to the authors, the bactericidal effects of ginger essential oil appears to be due to its ability to disrupt the bacterial cell membrane. As such, it may also be useful in food preservation.
Another study13 found a 10% ginger extract effectively killed Streptococcus mutans, Candida albicans and Enterococcus faecalis, which are also implicated in the causation of oral infections. More than a dozen other bacteria are also vulnerable to its effects,14 as are a number of biofilms.15
Ginger is not suitable for children under age 2, and adults should not take more than 4 grams of ginger per day. Pregnant women are advised to cap their intake at 1 gram per day.16
Echinacea
Echinacea extract has antibacterial properties and is known to have been used by Native Americans for more than 400 years to treat wounds and infections. According to Mount Sinai Hospital,17 echinacea may be used to treat “urinary tract infections, vaginal yeast (candida) infections, ear infections (also known as otitis media), athlete’s foot, sinusitis, hay fever (also called allergic rhinitis), as well as slow-healing wounds.”
It’s also a popular remedy for upper respiratory infections, such as the common cold and flu. According to a 2021 study,18 a nanosized echinacea extract was found to have up to 16-fold higher antibacterial activity against multidrug-resistant Klebsiella pneumoniae strains, compared to regular extract.
Echinacea is available in many forms, including extracts, tinctures, tablets and capsules. As a general recommendation for infection, take it three times a day for a maximum of 10 days.19
Goldenseal
Like echinacea, goldenseal is often used for the prevention and alleviation of cold symptoms, and a number of products combining the two can be found. One of the main constituents of goldenseal is berberine, known for its potent antibacterial properties.
Berberine primarily kills gram-positive bacteria, including MRSA. Berberine is not the sole component responsible for goldenseal’s antimicrobial effects, however. Extract from the aerial portions of the plant also has potent antibacterial effects that cannot be attributed to berberine alone, which is primarily found in the roots. As explained in a 2011 paper:20
“We hypothesize that [aerial goldenseal] extracts contain efflux pump inhibitors that synergistically enhance the antimicrobial activity of berberine. Bacterial efflux pumps are membrane bound proteins that pump toxins out of bacterial cells.
Overexpression of efflux pumps contributes to the development of resistance in bacteria, including S. aureus. Inhibition of efflux pumps may enhance the effectiveness of antimicrobial agents that are substrates for these pumps, and decrease the minimum inhibitory concentration for the antimicrobials.”
According to Mount Sinai,21 goldenseal is not recommended for pregnant or breastfeeding women, and those with high blood pressure, liver disease or heart disease should discuss its use with their medical provider, as it can interfere with medications prescribed for these conditions. Potential adverse effects include irritation of the skin, mouth, throat and vagina, and increased sensitivity to sunlight.
Myrrh Oil
When an antibiotic fails to kill off all the bacteria, you can end up with nongrowing bacterial persister cells. While these persisters do not undergo genetic change to make them resistant to the antibiotic, they often end up forming biofilms and are a major cause of chronic low-grade infections.22
This is where myrrh oil really shines, as research23 shows it preferentially kills off these nongrowing persister cells, and do so without the risk of promoting resistance. As noted by the authors:
“We report here that myrrh has a strong and unique antibiotic activity preferentially against nongrowing bacteria, a property not found in any commercially available antibiotic.
This unique property, along with its low toxicity and less tendency of antibiotic resistance development, suggests that myrrh can be developed to be a promising and ideal antibiotic with lower dosage requirements.”
Other research suggests it may be useful in the treatment of respiratory infections, gingivitis,24 treatment-resistant trichomoniasis vaginalis25 (a sexually transmitted disease) and Lyme disease.26
Thyme Essential Oil
Thyme essential oil has antibacterial, antibiofilm, antiviral, antifungal and antiseptic properties, and has a history of use in the treatment of upper respiratory infections. Quality matters, however. As noted in the 2020 paper, “Thymol and Thyme Essential Oil — New Insights into Selected Therapeutic Applications”:
“… only standardized preparations of thyme herb and essential oil that meet the requirements of national pharmacopeias or European Pharmacopoeia X (Ph. Eur. X) are used for the production of medicines.
According to the Ph. Eur. X definition, thyme herb is described as whole leaves and flowers separated from the dried stems of Thymus vulgaris or Thymus zygis or their mixture with 12 mL/kg of minimum essential oil (EO) and minimum thymol and carvacrol contents of 40%.
Thyme EO is defined as a product of the steam distillation of fresh flowering aerial parts of one or a mixture of both species with 37% – 55% thymol and 0.5% – 5.5% carvacrol concentrations …
Thyme herb and its volatile oil have long been used for the treatment of upper respiratory tract infections, symptoms of bronchitis, parasitic infections, pruritus associated with dermatitis, bruises, and sprains. Nowadays, it is generally used as an expectorant in cough associated with cold and also in dentistry as a disinfectant.
It exerts an antibacterial effect on Gram-positive and Gram-negative bacteria and has antiviral (herpes simplex virus type I, human rhinoviruses and influenza viruses), antifungal, antioxidant, anti-inflammatory, and spasmolytic activity.
Although thyme volatile oil has cytotoxic properties in high concentrations and may cause intestinal cell damage when administered orally, no toxicity has been reported at commonly used doses, and it can be considered as a safe drug.
Skin administration in high concentrations may cause irritation. In rare cases, an allergic reaction can occur, manifesting as skin rash, bronchospasm, asthma attack, and anaphylaxis. Therefore, this EO is contraindicated in persons allergic to thyme or other plants from the Lamiaceae family due to a possible cross-reactivity.”
Oregano Oil
Oregano oil has shown effectiveness against bacteria such as Streptococcus mutans,27 which causes dental cavities, as well as 11 different multidrug-resistant bacteria, including Acinetobacter baumannii, Pseudomonas aeruginosa, and MRSA, and their biofilms.28
Tests have also confirmed that repeated use of oregano oil does not lead to resistance, which makes it a useful remedy in the treatment of wounds. As reported in a 2018 study in Frontiers in Microbiology:29
“While efficiently inactivating bacteria, there was no evidence of resistance development after up to 20 consecutive passages of representative bacterial strains in the presence of sublethal doses of oregano oil.
In vivo study using the third-degree burn wounds infected with PA01 or USA300 demonstrated that oregano oil, topically applied 24 h after bacterial inoculation, sufficiently reduced the bacterial load in the wounds by 3 log10 in 1 h …
This bactericidal activity of oregano oil concurred with no significant side effect on the skin histologically or genotoxicity after three topical applications of oregano oil at 10 mg/ml for three consecutive days.
The investigation suggests potentials of oregano oil as an alternative to antibiotics for the treatment of wound-associated infections regardless of antibiotic susceptibility.”
Clove Extract and Cranberries Combat UTIs
Two natural antimicrobials shown to be useful against urinary tract infections (UTIs) are clove extract and cranberry juice. A study30 comparing the antimicrobial activity of clove extract and commercial clove essential oil (both having standardized eugenol content) found the extract was far more effective.
The ethanolic clove extract exhibited broad-spectrum inhibition against both gram-negative and gram-positive UTI-causing pathogens such as Proteus mirabilis, Staphylococcus epidermidis, S. aureus, E. coli and K. pneumoniae.
Cranberry juice is perhaps one of the most well-known remedies against UTIs. As explained in the 2018 review “Cranberry Consumption Against Urinary Tract Infections”:31
“Cranberry antibacterial effects have extensively been studied in order to understand the molecular mechanisms of action of its bioactive components and their clinical benefits against UTIs …
Current clinical evidence clearly indicates a possible benefit overall from the use of cranberries against UTIs. Cranberry consumption may prevent bacterial adherence to uroepithelial cells, reducing UTI related symptoms.
Cranberry consumption could also decrease UTI related symptoms by suppressing inflammatory cascades as an immunologic response to bacterial invasion … At present, cranberry supplementation can safely be suggested as complementary therapy in women with recurrent UTIs.”
A Cochrane Database of Systematic Review32 published in April 2023 confirmed that cranberry products — including juice or capsules — reduced the risk of symptomatic, confirmed UTIs in several groups.
In children, the UTI risk was reduced by 54%, in patients at increased risk to UTIs due to a medical intervention such as radiation treatment the risk was lowered by 53%, and in women with a history of recurrent UTIs the risk was reduced by 26%.
Nebulized Hydrogen Peroxide for Respiratory Infections
It’s also worth remembering what I believe is the most effective remedy for upper respiratory infections (URIs). Many make the mistake of taking antibiotics for URIs, but they won’t work, as they only kill bacteria and URIs are typically caused by viruses. The video above has my latest recommendations on how to prepare the hydrogen peroxide/saline nebulization solution and equipment to use.
Over the last three years, I’ve interviewed Dr. Thomas Levy and Dr. David Brownstein about this remarkably effective, yet simple and inexpensive treatment option. Both treated COVID patients with nebulized peroxide with great success.33,34
In most cases, including severe ones, improvement is seen within just a few hours. To inactivate viruses with hydrogen peroxide, all you need is a face mask that covers your mouth and nose and a nebulizer that emits a fine mist with properly diluted food grade hydrogen peroxide.
The microscopic mist, like smoke or vapor, can be comfortably inhaled deep into your nostrils, sinuses and lungs. I recommend using a desktop nebulizer, as they’re stronger and provide a much finer mist than handheld battery-operated versions.
Hydrogen Peroxide Rapidly Inactivates Viruses
Hydrogen peroxide (H2O2) consists of a water molecule (H2O) with an extra oxygen atom (O2), and it is the additional oxygen atom that allows it to inactivate viral pathogens. Some of your immune cells produce hydrogen peroxide to destroy pathogens. By killing the infected cell, viral reproduction is stopped. So, hydrogen peroxide therapy aids your immune cells to perform their natural function more effectively.
Many studies have investigated the use of hydrogen peroxide against different pathogens. For example, a 2020 review35 of 22 studies found that 0.5% hydrogen peroxide effectively inactivated a range of human coronaviruses, including those responsible for SARS and MERS, within one minute of exposure.
According to Brownstein, all pathogens studied to date have been found to succumb to hydrogen peroxide, albeit at varying concentrations and for different amounts of exposure.
How to Properly Dilute the Peroxide
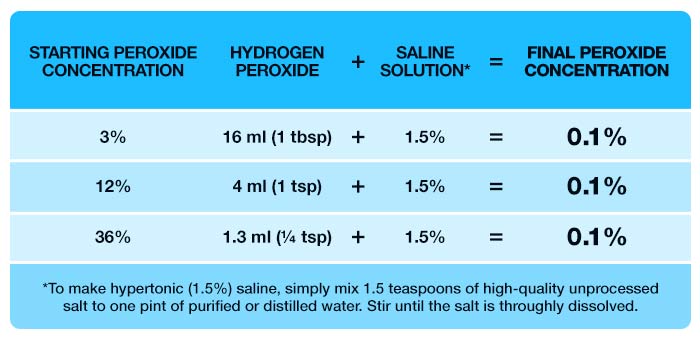
While you can use virtually any percentage of food grade peroxide, it’s crucial to dilute it properly before use. What you want is a 0.1% dilution, so even a 3% hydrogen peroxide will need to be diluted at least 30 times.
In a pinch, you could use commercial 3% hydrogen peroxide, the stuff used for wound care, but I don’t recommend routine use of it as it contains stabilizing chemicals that can detract from the benefits. Also, you want to dilute the hydrogen peroxide with hypertonic saline, not plain water, as the lack of electrolytes in the water can damage your lungs if you nebulize that. Using saline prevents the osmotic differential that can damage lung cells.
To end up with a final peroxide/hypertonic saline solution concentration of 0.1%, you need to go through two steps:
- Create the hypertonic saline solution
- Dilute the peroxide
I used to recommend using normal saline, which contains 0.9% salt, but a 2021 study36 found that a 1.5% sodium chloride solution (hypertonic saline) achieved a 100% inhibition of SARS-CoV-2 replication in vitro (in cell culture). Using lower levels of saline, like 1.1%, only inhibited 88%. So, I now recommend using hypertonic saline instead, which would be slightly less than double the amount of salt used to make normal saline.
To make hypertonic (1.5%) saline, simply mix 1.5 teaspoons of high-quality unprocessed salt to one pint of purified or distilled water. Stir until the salt is thoroughly dissolved. Be sure to use proper measuring spoons and not a regular kitchen teaspoon. For even greater precision, you could use a digital scale to measure out exactly 7.1 grams of salt.
If the 1.5% hypertonic solution causes nasal burning, irritation or cough, you can lower the concentration to 0.9% salt, which is isotonic normal saline. For this you would decrease the salt to one level teaspoon to one pint of water. Once you have your saline solution and a food grade hydrogen peroxide, dilute the peroxide according to the following chart, based on the concentration you’re starting with.
!WARNING:
Food grade peroxide at concentrations of 12% and 36% should NEVER be used full-strength either topically or internally. It MUST be diluted or severe injury can occur. Your safest bet is to use 3% food grade peroxide and dilute it as indicated so you end up with a solution of 0.1%.
Once you have your peroxide-saline solution, simply pour 1 teaspoon of it into the nebulizer and inhale the entire amount. If you like, you can add one drop of 5% Lugol’s iodine solution to the nebulizer as well. Some find it boosts the effects.
I recommend using nebulized peroxide for any suspected respiratory infection, and the earlier you start, the better. If you’re already presenting with a runny nose or sore throat, use the nebulizer for 10 to 15 minutes four times a day until your symptoms are relieved.
You can also use nebulized hydrogen peroxide for prevention and maintenance, which may be advisable during flu season. There is no danger in doing it every day if you’re frequently exposed, and there may even be additional beneficial effects, such as a rapid rise in your blood oxygen level.
