READ FULL PDF florida-surgeon-general-promotes-vitamin-d-for-covid-pdf
STORY AT-A-GLANCE
- Dr. Joseph Ladapo was appointed Florida surgeon general and secretary of the Florida Department of Health by Gov. Ron DeSantis September 21, 2021
- Ladapo has now issued a statewide public service announcement in support of commonsense COVID prevention strategies such as optimizing your vitamin D, staying active, eating nutrient-dense foods and boosting your immune system with supplements such as vitamin C, quercetin and zinc
- Florida Health even highlights emerging treatments such as fluvoxamine and inhaled budesonide. Importantly, Florida Health now states that “Physicians should use their clinical judgment when recommending treatment options for patients’ individualized health care needs. This may include emerging treatment options with appropriate patient informed consent, including off-label use or as part of a clinical trial”
- Despite publishing a scientific review on vitamin D for COVID in the peer-reviewed journal Nutrients, and the paper being the second most downloaded article this year, I’ve been vilified and targeted by the U.S. Food and Drug Administration and the Federal Trade Commission for reporting its benefits
- The evidence for vitamin D against COVID-19 satisfies Hill’s criteria for causality in a biological system, and dozens of studies have demonstrated vitamin D helps reduce all risks associated with COVID
As a ray of hope in what appears to be an utterly broken medical system, Florida’s new surgeon general, Dr. Joseph Ladapo, has issued a statewide public service announcement in support of commonsense COVID prevention strategies such as optimizing your vitamin D, staying active, eating nutrient-dense foods and boosting your immune system with supplements.
The HealthierYouFL.org website1 now urges Floridians to “Talk to your health care provider about how certain supplements or foods containing vitamins and minerals might help boost your immune system, such as zinc, vitamin D, vitamin C and quercetin.” These are all well-known supplements that have been shown to have a positive impact on your COVID-19 risk.
The surgeon general also supports the use of monoclonal antibodies in acute cases, and as prevention in high-risk patients who have been exposed to COVID-19. Available treatment locations can be found on FloridaHealthCOVID19.gov.
‘Physicians Should Use Clinical Judgment’
Florida Health even highlights emerging treatments such as fluvoxamine and inhaled budesonide. Importantly, Florida Health now states that:2
“Physicians should use their clinical judgment when recommending treatment options for patients’ individualized health care needs. This may include emerging treatment options with appropriate patient informed consent, including off-label use or as part of a clinical trial.”
Well, no one could be happier about this than I. I’ve been calling for vitamin D recommendations since the earliest days of the pandemic — ideally nationwide, but statewide is at least a start, especially considering Florida is the sunshine state. Instead, I’ve been vilified and targeted by the U.S. Food and Drug Administration and mainstream media for reporting its benefits.3,4
The FDA specifically mentioned Vitamin C, Vitamin D and Quercetin in their warning letter. Now that the Florida surgeon general agrees, will they also be warned by the federal authorities?
Ladapo was appointed Florida surgeon general and secretary of the Florida Department of Health by Gov. Ron DeSantis September 21, 2021,5 and it’s refreshing to finally see COVID guidance that makes sense. In his acceptance speech, Ladapo said:6
“I am honored to have been chosen by Governor DeSantis to serve as Florida’s next Surgeon General. We must make health policy decisions rooted in data and not in fear …
I have observed the different approaches taken by governors across the country and I have been impressed by Governor DeSantis’ leadership and determination to ensure that Floridians are afforded all opportunities to maintain their health and wellness, while preserving their freedoms as Americans.”
Vitamin D Papers Top List of Most Popular Studies of the Year
October 31, 2020, I published a scientific review7 in the journal Nutrients, co-written with William Grant, Ph.D., and Dr. Carol Wagner, both of whom are part of the GrassrootsHealth expert vitamin D panel.
As of October 31, 2021, our paper, “Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity” — which you can download and read for free — was the second most downloaded study from this journal in the past 12 months. It was also No. 2 in citations and No. 4 for views.
The study with the most downloads in the past year and the all-time highest number of views was another vitamin D paper8 by Bhattoa et.al., which found vitamin D supplementation reduced the risk of influenza and COVID-19 infections and deaths. The coauthors of my paper, Grant and Baggerly, were coauthors on this paper as well.
A third vitamin D paper, by Annweiler et.al., also nabbed the No. 1 spot for most-cited study in the past 12 months. This study found vitamin D supplementation improved survival in frail elderly hospitalized with COVID-19.
Clearly, vitamin D has been on the forefront of many minds, and I’m glad the Florida surgeon general recognizes its importance as well. While mainstream media and many so-called health authorities still hold on to the ridiculous claim that there’s “no scientific basis” for the recommendation of vitamin D for COVID, that is just false.
As early as the end of September 2020, data from 14 observational studies — summarized in Table 1 of our paper9 — showed that vitamin D blood levels are inversely correlated with the incidence and/or severity of COVID-19. Many critics of vitamin D will claim that these associations are not causal. However, there are statistical tools such as Bradford Hill that can actually prove causation through these associations are strong enough.
The Bradford Hill criteria are a group of nine principles (i.e., strength of association, consistency of evidence, temporality, biological gradient, plausibility or mechanism of action, and coherence, although coherence still needs to be verified experimentally) that can be useful in establishing epidemiologic evidence of a causal relationship between a presumed cause and an observed effect.
It has been widely used in public health research and has determined that the vitamin D insufficiency for COVID is indeed causal.10
How Vitamin D Protects Against COVID
It’s important to realize that your body is well-equipped to handle just about any infection, provided your immune system is working properly, as that is your body’s first line of defense. Vitamin D receptors are found in a large number of different tissues and cells, including your immune cells. This means vitamin D plays an important role in your immune function specifically.
If vitamin D is lacking, your immune system will be impaired, which in turn makes you more susceptible to infections of all kinds, including COVID-19. As explained in our paper, having sufficient vitamin D in your system can reduce your risk of COVID-19 and other respiratory infections through several different mechanisms, including but not limited to the following:11
| Reducing the survival of viruses |
| Inhibiting the replication of viruses12 |
| Reducing inflammatory cytokine production |
| Maintaining endothelial integrity (endothelial dysfunction contributes to vascular inflammation and impaired blood clotting, two hallmarks of severe COVID-19) |
| Increasing angiotensin-converting enzyme 2 (ACE2) concentrations — Angiotensin II is a natural peptide hormone that increases blood pressure by stimulating aldosterone. ACE2 normally consumes angiotensin I, thereby lowering the concentration of angiotensin II. However, SARS-CoV-2 infection downregulates ACE2, resulting in excessive accumulation of angiotensin II, which worsens the infection |
| Boosting your overall immune function by modulating your innate and adaptive immune responses |
| Reducing respiratory distress13 |
| Improving overall lung function |
| Helping produce surfactants in your lungs that aid in fluid clearance14 |
| Boosting T cell immunity, which plays an important role in your body’s defense against viral and bacterial infections. When vitamin D signaling is impaired, it significantly impacts the quantity, quality, breadth and location of CD8 T cell immunity, resulting in more severe viral and bacterial infections.15
According to a December 11, 2020, paper,16 high-quality T cell response actually appears to be far more important than antibodies when it comes to providing protective immunity against SARS-CoV-2 specifically |
| Increasing expression of antimicrobial peptides in your monocytes and neutrophils — both of which play important roles in COVID-19 |
| Enhancing expression of an antimicrobial peptide called human cathelicidin, which helps defend respiratory tract pathogens |
From my perspective, vitamin D optimization is one of the easiest, least expensive and most impactful strategies to reduce your risk of serious SARS-CoV-2 infection and other respiratory infections.
Vitamin D optimization is particularly important for dark-skinned individuals (who tend to have lower levels than Caucasians unless they spend extended time in the sun), the elderly, and those with preexisting chronic health conditions. All of these are also risk factors for COVID-19, so population-wide optimization of vitamin D levels could significantly improve COVID outcomes among the most vulnerable.
How Vitamin D Influences Your COVID Risks
At this point, there’s no shortage of studies showing higher vitamin D levels beneficially impact all stages of COVID-19. It:
| Lowers your risk of testing positive for COVID — The largest observational study17 to date, which looked at data for 191,779 American patients, found that of those with a vitamin D level below 20 ng/ml (deficiency), 12.5% tested positive for SARS-CoV-2, compared to just 5.9% of those who had an optimal vitamin D level of 55 ng/ml or higher. This inverse relationship persisted across latitudes, races/ethnicities, sexes and age ranges. |
| Reduces your risk of symptomatic illness — SARS-CoV-2-specific investigations have found that COVID-19 is far more common in vitamin D deficient individuals.
In one such study,18,19,20 82.2% of COVID-19 patients tested were deficient in vitamin D, compared to 47.2% of population-based controls. (Mean vitamin D levels were 13.8 ± 7.2 ng/ml, compared to 20.9 ± 7.4 ng/ml in controls.) They also found that blood levels of vitamin D were inversely correlated to D-dimer levels (a measure of blood coagulation). Many COVID-19 patients have elevated D-dimer levels, which are associated with blood clots. This was particularly true with the original SARS-CoV-2 virus, but while less common with subsequent variants, some blood clotting, just less intense, can still occur. |
| Reduces infection severity — Our vitamin D paper21 also lists data from 14 observational studies that show vitamin D blood levels are inversely correlated with the incidence and/or severity of COVID-19. This is quite logical, considering vitamin D regulates inflammatory cytokine production — a lethal hallmark of COVID-19 — and is an important regulator of your immune system. |
| Reduces your risk of hospitalization — Reduced severity would translate into a lower risk for hospitalization, and that’s precisely what researchers have found.
A Spanish study22,23 found baseline vitamin D levels inversely correlated with the risk of ICU admission, and that giving supplemental vitamin D3 (calcifediol at 532 micrograms on the first day of admission followed by 266 mcg on days 3, 7, 15 and 30) to hospitalized patients with PCR-confirmed COVID-19 reduced ICU admissions by 82%. |
| Reduces your risk of death — COVID-19 patients with a vitamin D level between 21 ng/mL (50 nmol/L) and 29 ng/mL (75 nmol/L) had a 12.55 times higher risk of death than those with a level above 30 ng/mL in one study.24 Having a level below 20 ng/mL was associated with a 19.12 times higher risk of death.
Another study25,26 found the risk of severe COVID-19 and related deaths virtually disappeared when vitamin D levels were above 30 ng/mL (75 nmol/L). A third paper27 found a marked variation in mortality depending on whether the patients lived above or below 35 degrees North latitude. As noted by the authors, having adequate vitamin D “could be very important in preventing the cytokine storm and subsequent acute respiratory distress syndrome that is commonly the cause of mortality.”28 |
| Speeds viral clearance — While having enough vitamin D in your system will reduce your odds of infection and serious illness, taking oral vitamin D once infected can still help you recover faster.
Research29 published in November 2020 found oral vitamin D supplementation in SARS-CoV-2-positive individuals with mild symptoms who also had low vitamin D, helped speed up viral clearance. Participants were randomly assigned to receive either 60,000 IUs of oral cholecalciferol (nano-liquid droplets) or a placebo for seven days. The target blood level was 50 ng/mL. Anyone who had not achieved a blood level of 50 ng/mL after the first seven days continued to receive the supplement until they reached the target level. Periodically, all participants were tested for SARS-CoV-2 as well as fibrinogen, D-dimer, procalcitonin and CRP, all of which are inflammatory markers. The primary outcome measure of the study was the proportion of patients testing negative for COVID-19 before Day 21 of the study, as well as changes in inflammatory markers. Of the 16 patients in the intervention group, 10 (62.5%) tested negative by Day 21, compared to just five of the 24 controls (20.8%). Fibrinogen levels were also significantly decreased in the treatment group, indicating lower levels of clotting. |
How to Optimize Your Vitamin D Level
For optimal health, immune function and disease prevention, you want a vitamin D blood level between 60 ng/mL and 80 ng/mL year-round. In Europe, the measurements you’re looking for are 150 nmol/L and 200 nmol/L.
If you live in a sunny locale like Florida and practice sensible sun exposure year-round, you might not need any supplements. The DMinder app30 is a helpful tool to see how much vitamin D your body can make depending on your location and other individual factors.
Many, unfortunately, don’t get enough sun exposure for one reason or another, and in these cases, an oral vitamin D supplement may be required. Just remember that the most important factor here is your blood level, not the dose, so before you start, get tested so you know your baseline.
Here’s a summary of how to determine whether you might need an oral supplement, and your ideal dosage:
1. First, measure your vitamin D level — One of the easiest and most cost-effective ways of measuring your vitamin D level is to participate in the GrassrootsHealth’s personalized nutrition project, which includes a vitamin D testing kit. Once you know what your blood level is, you can assess the dose needed to maintain or improve your level.
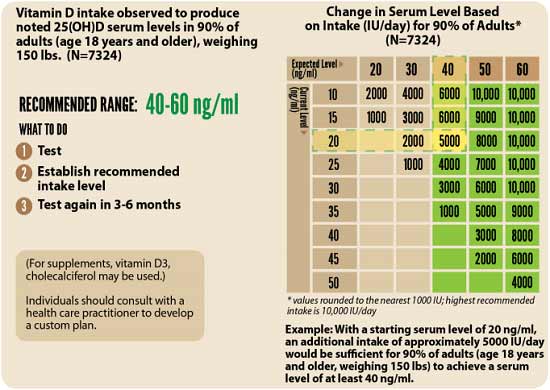
2. Assess your individualized vitamin D dosage — To do that, you can either use the chart below, or use GrassrootsHealth’s Vitamin D*calculator. (To convert ng/mL into the European measurement (nmol/L), simply multiply the ng/mL measurement by 2.5.) To calculate how much vitamin D you may be getting from regular sun exposure in addition to your supplemental intake, use the DMinder app.31
Factors that can influence your vitamin D absorption include your magnesium32 and vitamin K233 intake. Magnesium is required for the conversion of vitamin D into its active form.34,35,36,37 If your magnesium level is insufficient, the vitamin D you ingest orally may simply get stored in its inactive form.38,39
Research by GrassrootsHealth40 shows you need 146% more vitamin D to achieve a blood level of 40 ng/ml (100 nmol/L) if you do not take supplemental magnesium, compared to taking your vitamin D with at least 400 mg of magnesium per day.
Your best bet is to take your vitamin D with both magnesium and K2. According to GrassrootsHealth,41 “combined intake of both supplemental magnesium and vitamin K2 has a greater effect on vitamin D levels than either individually,” and “those taking both supplemental magnesium and vitamin K2 have a higher vitamin D level for any given vitamin D intake amount than those taking either supplemental magnesium or vitamin K2 or neither.”
Data42 from nearly 3,000 individuals revealed 244% more oral vitamin D was required to get 50% of the population to achieve a vitamin D level of 40 ng/ml (100 nmol/L) if they weren’t concurrently also taking magnesium and vitamin K2.
3. Retest in three to six months — Remeasure your vitamin D level in three to six months, to evaluate how your sun exposure and/or supplement dose is working for you.
4. Take activated vitamin D (calcitriol) if your level is low and you come down with an acute infection like COVID. The dose is 0.5 mcg on day one and then 0.25 mcg daily for seven days.
